Introduction

Common symptoms of conjunctivitis
Conjunctivitis (commonly known as pink eye) is a very common eye condition that can affect people of all ages—from newborns to the elderly. It can be caused by viruses, bacteria, allergies, or irritants. Typical symptoms include red eyes, swelling, itching, discharge, and excessive tearing.
Eye drops are the first-line treatment choice, helping to relieve symptoms and support recovery. However, each type of drop has its own role and must be used correctly as prescribed.
Common causes of conjunctivitis
Conjunctivitis is an inflammation of the conjunctiva causing redness, itching, tearing, sometimes with discharge. The common causes include:
- Viral conjunctivitis: the most common, accounting for up to 90% of cases, highly contagious.
- Bacterial conjunctivitis: produces purulent discharge, sticky eyelids, and spreads easily.
- Allergic conjunctivitis: non-contagious, often seen in those allergic to pollen, dust, or animal dander.
Commonly used eye drops
1) Artificial tears
Products such as Sanlein, Systane Ultra, Refresh Tears… help soothe and reduce irritation. They can be used multiple times a day (4–10 times).
Function: Moisturizes, washes away debris, reduces dryness and discomfort. However, they only relieve symptoms and do not kill the viruses or bacteria causing the disease.
Note: Prefer preservative-free types if frequent use is required or in patients with chronic dry eye. Safe for children and pregnant women.
2) Antibiotic eye drops
Examples: Tobramycin (Tobrex), Polymyxin/Trimethoprim, Ciprofloxacin… Used for bacterial conjunctivitis. Only use with a doctor’s prescription to avoid antibiotic resistance.
Function: Kills bacteria causing conjunctivitis, shortens the duration of illness.
Note: Only effective in bacterial conjunctivitis (usually with yellow/green pus). Ineffective for viral or allergic conjunctivitis. Misuse can cause antibiotic resistance.
3) Antiviral eye drops
Example: Trifluridine (Viroptic), usually prescribed in herpes simplex virus infection with risk of corneal ulceration.
Function: Inhibits viral replication (especially HSV). Helps prevent corneal ulcer complications.
Note: Must be closely monitored by an ophthalmologist, and not used for longer than 21 days. Possible side effects: irritation, temporary blurred vision.
4) Antihistamine eye drops
Ketotifen, Bepotastine, Emedastine… help relieve itching and tearing in allergic conjunctivitis.
Note: Most effective when combined with allergen avoidance (pollen, dust, animal dander). Maintain intervals when combined with other eye drops. Do not overuse without medical supervision.
5) Topical corticosteroids
Loteprednol, Dexamethasone, Prednisolone… are strong anti-inflammatory agents.
Function: Rapidly reduces inflammation, controls swelling and redness in severe cases.
Note: Should only be used in severe cases under strict medical supervision due to risks of glaucoma, cataracts, or opportunistic infections. Recommended for short-term use with follow-up exams.
Eye drops: Primary role in treatment

Using eye drops correctly to treat conjunctivitis
Eye drops are considered the frontline treatment for conjunctivitis. Each type works differently depending on the cause:
| Eye drop group | Main function | Usage note |
|---|---|---|
| Antibiotics | Treats bacterial conjunctivitis, reduces purulent discharge | Only with doctor’s prescription, avoid resistance |
| Antivirals | Used in viral conjunctivitis | Rarely used, often combined in protocols |
| Antihistamines/mast cell stabilizers | Reduce itching, tearing due to allergies | Do not overuse, avoid overdosing |
| Corticosteroids | Strong anti-inflammatory | Strict monitoring required, risk of glaucoma, cataracts |
| Artificial tears | Moisturizes, reduces irritation | Safe for long-term use |
How to use eye drops properly
- Wash hands before use.
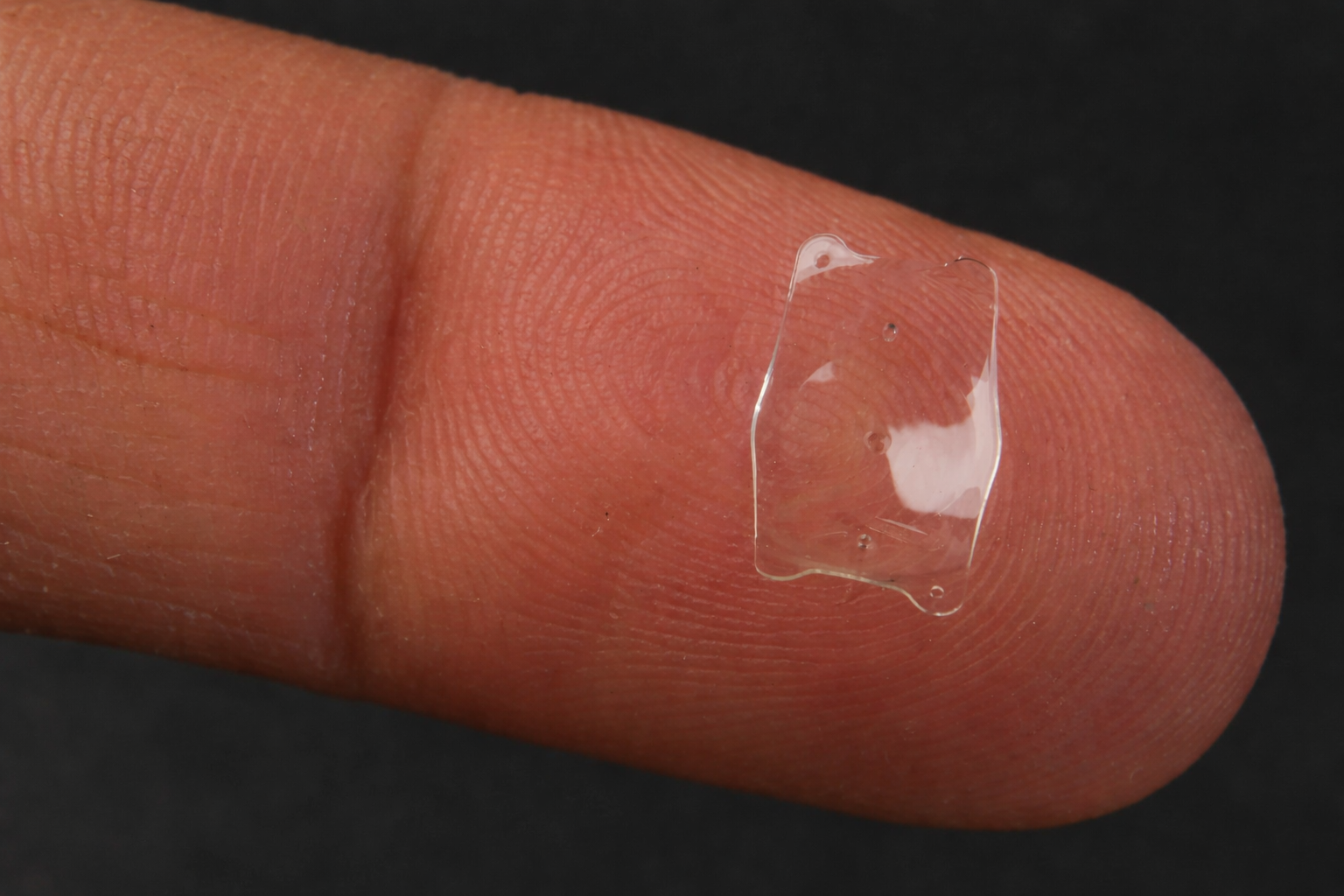
- Remove contact lenses (if any).
- Tilt head back, pull lower eyelid, instill prescribed drops.
- Close eyes and press inner corner gently for absorption.
- Wipe excess liquid with a clean tissue.
- If using multiple drops, wait at least 3–5 minutes.
Common mistakes when using eye drops
Although common, many patients still make mistakes when using eye drops:
- Self-purchasing corticosteroid drops without prescription.
- Sharing eye drop bottles, increasing infection risk.
- Not following dosage and frequency instructions.
- Using too many types at once, causing irritation or interactions.
According to Medlatec, misuse of corticosteroids may cause severe complications such as glaucoma or corneal ulcers.
Comprehensive treatment: When to go beyond eye drops?

Cold compress helps reduce swelling and discomfort
In most cases, eye drops help control symptoms. However, if the condition persists or recurs, the doctor may suggest advanced measures:
- Cold compresses or saline rinses.
- Maintain hygiene, avoid rubbing eyes, change pillowcases frequently.
- Wear protective glasses when swimming or working in dusty environments.
When to see a doctor?
Seek immediate ophthalmology consultation if you experience:
- Severe eye pain, light sensitivity.
- Sudden blurred vision.
- Thick yellow-green discharge.
- No improvement after 5–7 days of prescribed treatment.
Conclusion
Eye drops play a vital role in treating conjunctivitis, helping to reduce inflammation, control symptoms, and prevent complications. However, proper use—correct type, dose, and indication—is essential. Patients should not self-medicate but seek professional ophthalmologic diagnosis and treatment.

 vi
vi 12-Sep-2025
12-Sep-2025










 0916.741.763
0916.741.763 Appointment
Appointment