How many times can you undergo myopia surgery?
Close-up of eyes after successful myopia surgery
If you have ever thought about having vision correction surgery, you might have asked yourself: “How many times can I have myopia surgery?” It’s a common question, especially among people who have already undergone the procedure once but notice their vision changing again over time.
The truth is, while myopia surgery can deliver excellent and long-lasting results, it cannot be repeated indefinitely. Understanding the limitations, medical conditions, and recovery factors involved will help you make informed and safe decisions about your eyes.
In principle, the human eye should not be operated on too many times. Each surgical procedure, regardless of the technology or method used, affects the corneal structure or internal eye tissues to some extent. Therefore, ophthalmologists generally recommend that myopia surgery be performed only once, except in certain specific cases where a second enhancement may be medically appropriate.
In clinical practice, the procedure is usually performed only once. In some special cases, a second surgery (enhancement) may be considered if the eyes meet the required conditions — typically up to two times for most patients who have had corneal-based laser surgery. For other techniques (such as Phakic ICL implantation or lens replacement), additional interventions differ (for instance, ICL replacement) and must be carefully evaluated.
Patients aged between 18 and 40 are the best candidates for a second surgery if their vision regresses after the first one and the eye still meets the medical requirements. For patients over 40, doctors often advise against redoing the surgery immediately. Instead, they may recommend waiting until cataract signs appear so that a lens replacement surgery can correct both cataracts and residual refractive error at once — achieving better long-term results.
When is a second myopia surgery needed?
Doctors may recommend a second surgery in the following cases:
- Recurrent myopia (residual myopia) or residual refractive error that causes discomfort and affects vision quality. Although the recurrence rate after laser surgery is low, it still occurs in some cases.
- The eyes meet all safety criteria: the cornea remains sufficiently thick, corneal topography is stable, there are no signs of progressive corneal disease (such as keratoconus), and refraction has been stable for 6–12 months prior to the second procedure.
- Age: younger patients (under 40) may be considered for a second surgery if their eye condition is suitable; for patients over 40, presbyopia or early cataracts should be considered — in some cases, lens replacement can address both myopia and presbyopia at once.
Essential conditions before undergoing a second myopia surgery

Medical team performing myopia surgery in a modern operating room
Before being approved for a second myopia surgery, you should:
- Have a detailed eye examination: corneal topography, epithelial/corneal thickness measurement, intraocular testing (retinal OCT), and endothelial cell density measurement.
- Ensure stable refraction (changes ≤ ±0.5D within 6–12 months).
- Maintain sufficient corneal tissue for additional intervention (for laser surgery). If the cornea is too thin, the doctor may recommend PRK/TransPRK or an Phakic ICL instead of further corneal ablation.
- Ensure there are no active eye diseases (inflammation, uncontrolled glaucoma, severe retinal conditions) and that overall eye health is stable.
If the cornea is too thin after the first procedure, your doctor may advise against another laser surgery and instead suggest alternative treatments, such as PRK/TransPRK (which removes surface tissue without creating a corneal flap) or Phakic ICL lens implantation — an advanced, reversible solution suitable for patients with thin corneas or high degrees of myopia.
Which method is used for secondary myopia correction?
- Laser enhancement (recreating the LASIK flap or performing PRK/TransPRK) if the cornea is thick enough and the surface is stable.
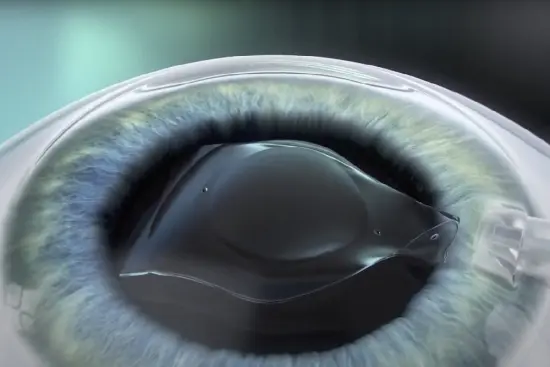
- Switching methods: if corneal tissue is insufficient, Phakic ICL (Phakic ICL) implantation may be considered — ideal for patients with high myopia or thin corneas. The ICL can be safely removed in the future if necessary.
- Lens replacement (RLE / IOL) for older patients showing signs of presbyopia or early cataract — this option corrects myopia and addresses lens opacity in a single procedure.
Each technique has distinct benefits and risks, so consultation with an experienced refractive surgeon is essential before making a decision.
Increased risks of a second myopia surgery

Doctor performing myopia surgery on a patient
While myopia surgery in general is safe, repeating it carries slightly higher risks compared to the first operation. Some potential complications include:
- Dry eye syndrome: The corneal nerves take longer to recover, causing discomfort or blurred vision.
- Corneal irregularities: Excessive thinning or uneven healing may cause astigmatism or decreased visual quality.
- Endothelial cell damage: Can increase the risk of corneal swelling, especially if an intraocular lens was implanted.
- Infection or inflammation: Though rare, improper hygiene or non-compliance with postoperative care can cause serious eye infections.
To minimize these risks, it is crucial to undergo surgery only at certified eye hospitals equipped with modern technology and experienced refractive surgeons.
Postoperative care — especially after the second surgery
- Strictly follow the prescribed medication regimen (antibiotics, anti-inflammatory drops, artificial tears).
- Avoid rubbing your eyes, heavy physical activity, swimming, or saunas for at least two weeks.
- Wear protective glasses when needed during the first two weeks.
- Attend all follow-up visits so your doctor can monitor intraocular pressure, endothelial cell health, and refractive stability.
In short: myopia surgery should typically be performed once; in specific cases, a second procedure may be considered — up to approximately two times (for corneal-based laser surgery). The decision depends on your initial surgical method, corneal thickness, age, and current eye condition.
If you are considering another procedure, visit a reputable ophthalmology center, undergo a full diagnostic evaluation, and consult your doctor about the most suitable option (laser enhancement, PRK, ICL, or RLE), the potential benefits and risks, and the long-term follow-up plan.

 vi
vi 03-Nov-2025
03-Nov-2025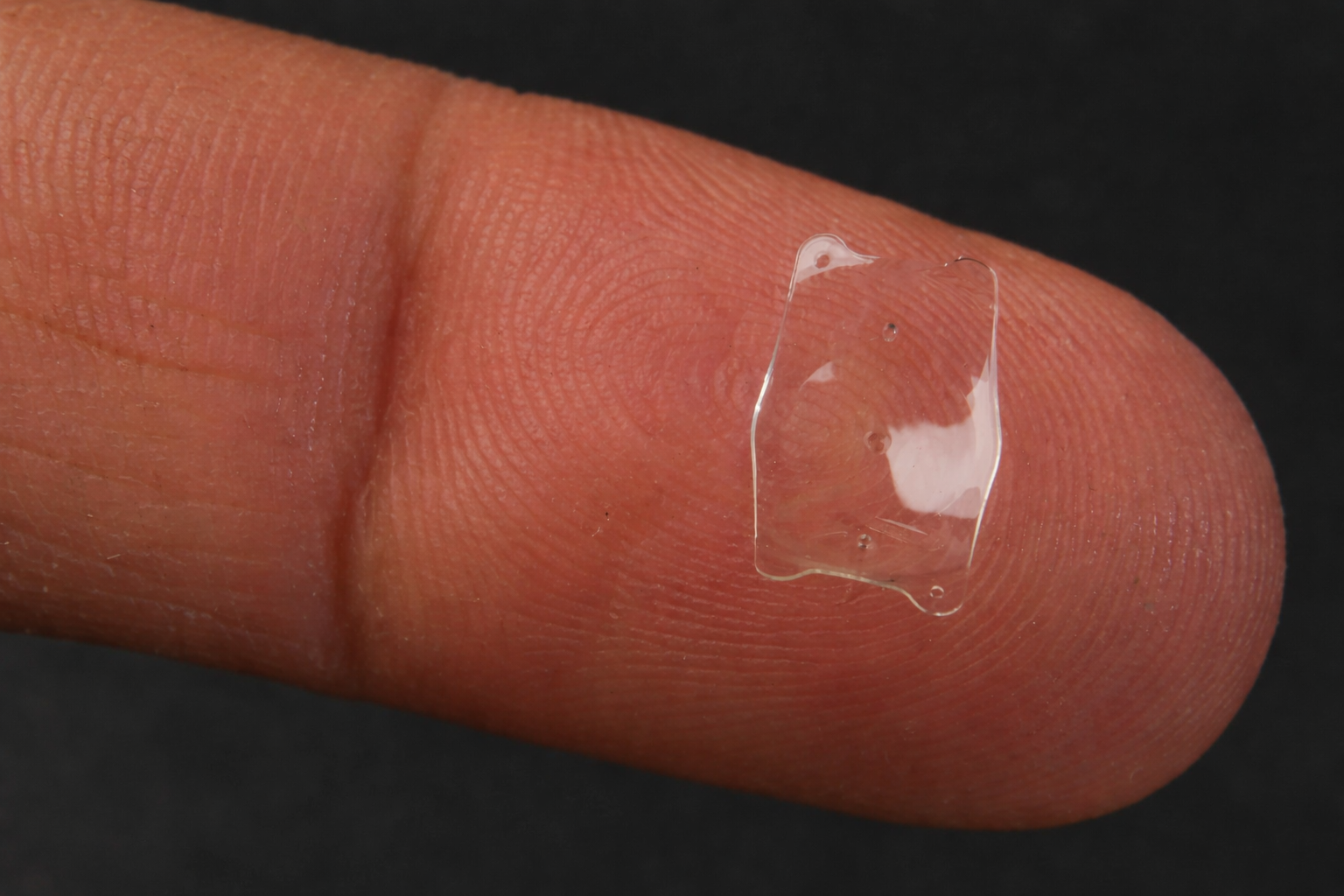










 0916.741.763
0916.741.763 Appointment
Appointment