Introduction

Is a thin cornea a medical condition?
The cornea is the transparent tissue at the front of the eye. It acts like a “window” that lets light in and helps focus images sharply on the retina. Normally, the average corneal thickness is about 500–550 micrometers. When the thickness is below this range, the condition is called a thin cornea.
A thin cornea not only affects whether you are a candidate for certain refractive procedures but also carries higher risks for several serious eye problems. So what is a thin cornea, what causes it, and how do you recognize the symptoms?
What is a thin cornea?
A thin cornea means the corneal thickness is lower than normal, typically <500 micrometers. When the cornea is too thin, laser procedures (LASIK, PRK) may be unsafe because they can weaken the cornea and lead to corneal ectasia (keratectasia).
This is not necessarily a separate disease; it is often a sign related to ocular structure or a complication of an existing condition.
Causes of a thin cornea
A thin cornea can arise from several factors:
| Cause group | Details |
|---|---|
| Congenital | Some people are born with a thin cornea, often related to genetic factors. |
| Corneal diseases | For example, keratoconus, in which the cornea becomes both thinner and protrudes forward. |
| Previous surgery | Laser procedures (LASIK, PRK) can progressively thin the cornea over time. |
| High refractive error | People with high myopia or astigmatism may have a congenitally thinner cornea. |
| Trauma/inflammation | Chronic infection or inflammation can weaken and thin the cornea. |
Common symptoms
A thin cornea does not always cause obvious symptoms. However, pay attention if you experience:
- Blurred vision that does not improve much with glasses.
- Distorted vision or light scatter, especially at night.
- Light sensitivity and glare.
- Eye strain or ache with prolonged tasks.
- Frequent dryness or discomfort in some cases.
Does a thin cornea affect vision?
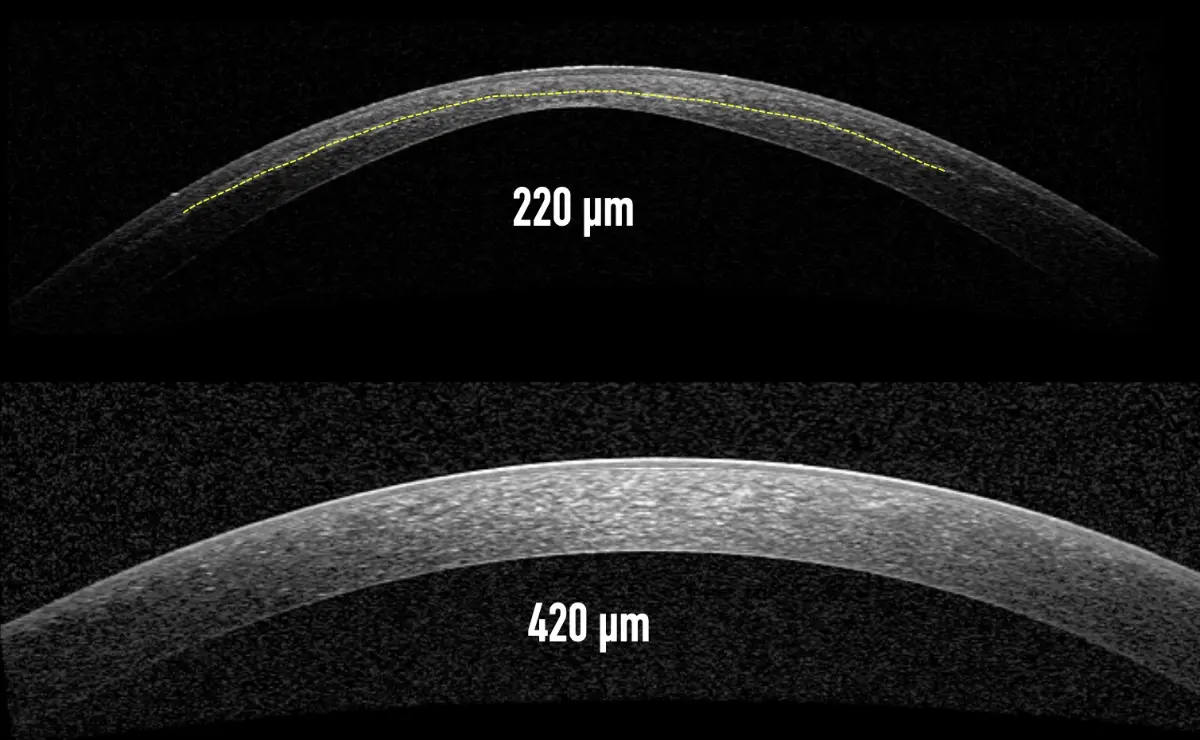
Comparing corneal thickness on cross-section imaging
In reality, thickness alone does not determine whether the cornea is “strong.” Corneal stability depends on the internal network of horizontally oriented collagen fibers. If these cross-linkages are robust, a cornea may be thin yet structurally stable; if the linkages are weak, the cornea can deform and lose strength.
Even so, a thin cornea carries more risk because it sits at the outermost layer of the eye and constantly bears intraocular pressure. When it becomes too thin, its load-bearing capacity drops, increasing the chance of surface deformation and reduced visual quality.
Risk of regression after laser surgery
Laser procedures like LASIK flatten the cornea to correct refractive error. If the cornea is already thin, intraocular pressure can bow it forward again after surgery, causing rapid myopic regression and unstable outcomes. For this reason, many patients with thin corneas are not eligible for LASIK/PRK.
Persistent dry eye
Thin corneas tend to be more steeply curved, especially centrally. This makes it harder for the tear film to spread evenly, leading to chronic dry eye. Typical complaints include blurred vision, burning, foreign-body sensation, discomfort with prolonged screen time, and worse night vision.
Corneal ectasia (keratoconus)
This is the most serious complication in people with very thin corneas. The cornea gradually thins and bulges irregularly, bending light abnormally and producing distorted, blurry images with significant visual loss. There is currently no treatment that fully reverses this; standard spectacles cannot correct it because they cannot compensate for the irregular shape.
Is a thin cornea dangerous?
If undetected or not monitored, a thin cornea can lead to serious visual problems, including:
-
Risk of corneal ectasia after laser surgery.
-
Difficulty selecting a suitable surgical method to correct myopia/astigmatism.
-
Greater chance of long-term visual instability.
-
Higher susceptibility to damage from ocular trauma.
Therefore, measuring and assessing corneal thickness is a mandatory step before any refractive procedure.
Diagnostic methods

Modern corneal topography system helps doctors precisely assess corneal thickness and shape before treatment.
Determining corneal thickness cannot be done at home; it requires specialized equipment at an eye clinic or hospital. Ophthalmologists often combine multiple techniques to ensure accuracy:
- Corneal Topography: Evaluates the cornea’s shape, curvature, and thickness in detail from the periphery to the center.
- Pachymetry: Measures central corneal thickness using ultrasound or modern optical technology to minimize error.
- Endothelial cell count: Checks endothelial cell density and central corneal thickness to assess long-term corneal health.
- Auto-refractor: Measures refractive parameters and provides an average corneal thickness reading.
- Comprehensive eye exam: Rules out associated conditions such as keratoconus, corneal scars, and glaucoma.
By combining these assessments, doctors can accurately evaluate your corneal status and recommend the safest, most suitable treatment or surgical plan.
Refractive solutions for thin corneas
There is no medication that makes the cornea thicker, but patients still have several safe options to correct refractive errors:
1. Eyeglasses or contact lenses
- A simple solution without surgery.
- However, many people find lifelong dependence on lenses inconvenient.
2. PRK (Photorefractive Keratectomy)
- Removes the corneal epithelium instead of creating a flap like LASIK.
- More suitable for thinner corneas, though recovery takes longer.
Phakic ICL
- Does not damage the cornea because no corneal tissue is cut.
- FDA-recognized and safe for patients with thin corneas, dry eyes, or high myopia.
- Procedure time is only 20–30 minutes, with fast recovery and no dry-eye induction.
- It can be removed later if necessary.
Quick comparison:
| Criteria | LASIK/PRK | Phakic ICL |
|---|---|---|
| Impact on cornea | Yes (tissue cutting) | No |
| Suitable for thin corneas | Limited | Highly suitable |
| Dry-eye risk | Higher | Lower |
| Visual recovery | Several days–weeks | Almost immediate |
| Removability | No | Removable |
A thin cornea is not immediately dangerous by itself, but it is a crucial factor affecting ocular health and refractive treatment options. Understanding the causes, symptoms, and appropriate solutions will help you protect your vision in the long run.

 vi
vi 19-Sep-2025
19-Sep-2025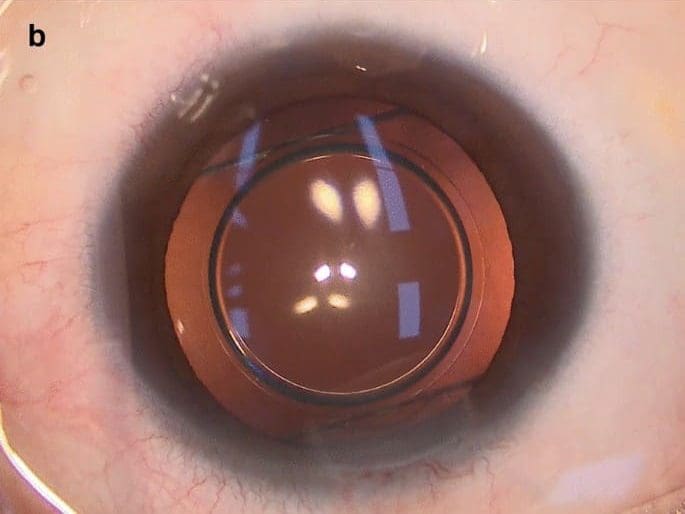












 0916.741.763
0916.741.763 Appointment
Appointment