Why Do Your Eyes Twitch? Causes, Types, and Treatment Solutions

Eye twitching is one of the most common conditions today
Eye twitching, also known medically as blepharospasm, involves involuntary, repeated contractions of the eyelid or surrounding muscles. While most cases are harmless, persistent or severe twitching may signal an underlying neurological or ocular condition. Understanding the causes, classifications, and treatments helps protect vision and quality of life.
Overview of Eye Twitching
Eye twitching is typically benign, painless, and may disappear on its own within minutes or days. However, when twitching persists for weeks and is accompanied by symptoms such as frequent squinting, light sensitivity, or difficulty opening the eyes, it may indicate a more complex neurological disorder or motor dysfunction of the eye.
- Approximately 10–15% of adults experience temporary eyelid twitching at some point.
- Middle-aged women may be affected more often than men, partly due to hormonal fluctuations and stress sensitivity.
- A minority of chronic cases are associated with central nervous system motor disorders and require medical evaluation.
Types of Eye Twitching
1. Mild Twitching
- Causes: fatigue, stress, insufficient sleep, or overuse of caffeine and alcohol.
- Characteristics: transient and usually resolves spontaneously within a few days.
- Associated factors: dry eye and corneal irritation, common among long-term contact lens wearers.
2. Benign Essential Blepharospasm
- Often appears in middle age and can gradually worsen over time.
- Symptoms include blurred vision, photosensitivity, and occasional eyelid drooping.
- Pathogenesis may involve dopamine neurotransmission dysfunction and genetic predisposition.
3. Hemifacial Spasm

Hemifacial spasm involves both the muscles around the mouth and eyelids
This rare spasm typically affects one side of the face and may involve both the eyelids and the perioral muscles.
- Primary cause: vascular compression of the facial nerve.
- Risks: without treatment, progressive facial asymmetry and psychological distress can occur.
Causes of Eye Twitching
Eye twitching can result from lifestyle factors, environmental triggers, medication effects, or neurological conditions. The table below summarizes common causes and mechanisms:
| Common Cause | Mechanism |
|---|---|
| Fatigue, stress | Overuse of extraocular and periocular muscles leading to uncontrolled contractions |
| Lack of sleep | Disruption in neurotransmission and reduced neuronal recovery |
| Caffeine, alcohol, tobacco | Overstimulation of the central nervous system |
| Dry eye, conjunctivitis | Increased ocular surface irritation and reflex blinking |
| Neurological disorders | Parkinson’s disease, dystonia, Bell’s palsy, Tourette’s syndrome |
| Medication side effects | Particularly anticonvulsants and strong sedatives altering neuromuscular signaling |
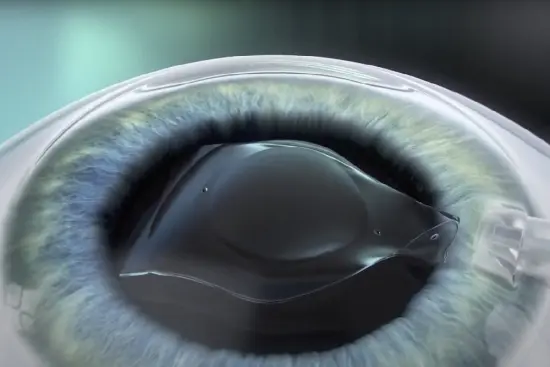
Note: Individuals with severe refractive errors (e.g., high myopia or astigmatism) often accommodate excessively, which may increase periocular muscle strain and predispose to twitching.
Treatment of Eye Twitching
Management depends on severity, frequency, triggers, and whether an underlying ocular or neurological condition is present. Options range from lifestyle optimization to medical and surgical interventions.
1. Lifestyle Adjustments and Home Care
- Adequate sleep: aim for 7–8 hours nightly to restore neural function and reduce spasms.
- Limit stimulants: reduce caffeine, alcohol, and tobacco to avoid central nervous system overactivation.
- Artificial tears: lubricate the ocular surface to prevent dry eye, a frequent twitching trigger.
- 20-20-20 rule: every 20 minutes of screen use, look 20 feet away for 20 seconds to relax accommodation.
- Gentle periocular massage: promotes blood flow and relieves muscle tension.
- Stress management: meditation, yoga, and controlled breathing help attenuate stress-driven twitching.
2. Medical Treatment

Visit a reputable medical facility for examination and diagnosis when experiencing eye twitching
- Botulinum toxininjections (Botox, Dysport, Xeomin): small doses injected into eyelid muscles can reduce contractions for 3–6 months; first-line for chronic blepharospasm.
- Sedatives or muscle relaxants: Clonazepam, Lorazepam, Trihexyphenidyl (Artane) may provide short-term relief; use only under medical supervision due to dependence and side-effect risks.
- Specialized eye drops: anti-inflammatory or antihistamine drops for coexisting dry eye, blepharitis, or allergic ocular disease.
- Surgical options:
- Myectomy: partial removal of orbicularis oculi fibers in severe, refractory blepharospasm.
- Microvascular decompression: indicated for hemifacial spasm caused by vascular compression of the facial nerve.
3. Supportive and Alternative Methods
- Acupuncture and biofeedback: may reduce symptoms in selected patients according to emerging evidence.
- Nutritional support:
- Omega-3 fatty acids: improve tear film stability and ocular surface comfort.
- B vitamins (B1, B6, B12): support neural conduction and neuromuscular health.
- Magnesium: participates in neuromuscular transmission; may help reduce spasms.
- Protective eyewear: blue-light–filter or tinted lenses to mitigate light sensitivity and digital eye strain.
Most episodes of eye twitching are transient signs of fatigue, stress, or lifestyle imbalance. Persistent or severe cases, especially those with facial involvement or functional vision impairment, warrant professional evaluation to exclude neurological or ocular disease.
An effective plan often combines sleep hygiene, stress control, and ocular surface care with targeted medical therapies. For chronic blepharospasm or hemifacial spasm, botulinum toxin injections and, in select cases, surgical intervention can significantly improve symptoms, function, and quality of life.

 vi
vi 22-Sep-2025
22-Sep-2025










 0916.741.763
0916.741.763 Appointment
Appointment