Signs of astigmatism in children often appear early but are easily overlooked because they resemble nearsightedness or ordinary eye strain. As a result, children experience blurred vision both near and far, with distorted or smeared text. Correctly identifying the signs of astigmatism helps parents detect it early, prevent amblyopia, and improve their child’s learning efficiency.
What is Astigmatism?
Blurred, overlapping images are one of the signs of astigmatism in children that parents need to pay attention to.
Astigmatism is a common refractive error that occurs when the cornea (the clear front surface of the eye) or the lens has an irregular curvature. Instead of focusing light onto a single point on the retina, the light rays are dispersed at multiple points, making images blurred or distorted.
Unlike myopia, which only causes blurred distance vision, astigmatism causes blurred vision both near and far. Many children with astigmatism also complain of stretched objects, tilted text, or ghosting.
5 signs parents should closely monitor
1) Children squint when looking far or near
Sign: The child often pulls their eyelids, squints when looking at the board, TV, or even when reading books at close distances. Some children say “vision is blurry, shadowy” or that they have to “strain” to see clearly.
Why it happens: Astigmatism prevents images from focusing on one point, instead spreading along the irregular curve of the cornea/lens. Squinting temporarily increases depth of field, improving clarity but causing eye fatigue.
- Parents can try: Have the child look at letters/numbers from 3–4 m away with decreasing sizes; observe how often they squint.
- When to see a doctor: If the child squints more than 3 times/day or continues for over 2 weeks.
2) Children tilt their head or rotate to see or read
Sign: When reading, the child often tilts their head to one side, rotates the notebook, or sits unevenly. When watching TV, the child finds a “preferred viewing angle.”
Mechanism: Tilting the head helps align the line of sight with the least distorted meridian, making the image clearer on the retina. This is a typical sign of irregular astigmatism by axis.
- Parents can try: Fix the book, change the light source; observe if the child turns their head/notebook to “focus.”
- When to see a doctor: If the habit persists for more than 1–2 weeks or is accompanied by neck and shoulder pain.
3) Eye rubbing, headaches, eye strain at the end of the day

Children who frequently rub their eyes, complain of headaches or fatigue – an early warning of astigmatism or other refractive errors.
Sign: Children often rub their eyes after school, complain of heavy eyelids, pain in the forehead-temple area, and become irritable when doing homework.
Cause: The accommodation system works harder to compensate for image distortion caused by astigmatism. Prolonged overload causes eye fatigue, dryness, headaches – especially after long reading/writing.
- Parents can try: The 20–20–20 rule (every 20 minutes of near work, look 20 feet ≈ 6 m away for 20 seconds); if symptoms improve, refractive error testing is needed.
- When to see a doctor: If headaches occur more than 2–3 times/week or require pain medication.
4) Poor concentration, slanted writing, misreading
Sign: The child’s writing is misaligned, spacing uneven; frequent confusion of similar letters/numbers (e.g., H–N, O–Q, 3–8). Teachers often report the child “copies slowly, writes incorrectly.”
Explanation: Astigmatism causes certain strokes to appear clearer than others; when shifting lines or changing font sizes, the eyes constantly adjust, leading to “slippage.”
- Parents can try: Give a short reading with decreasing font size; track reading/copying mistakes over time.
- When to see a doctor: Persistent mistakes despite proper practice.
5) Poor vision in dim light, stumbling at night
Sign: The child struggles when walking around the house at night, has trouble reading small signs/symbols in dark classrooms, or sees glare/halos around lights.
Reason: Pupils dilate in the dark, exposing more of the “irregular” cornea, increasing aberrations and glare/halo. This effect is more pronounced in children with astigmatism.
- Parents can try: “Bright spot” test (read reflective signs at 2–3 m in dim light); if frequent mistakes occur, consult an eye doctor.
- When to see a doctor: Any complaints of poor night vision lasting more than 1–2 weeks.
Comparison of signs: Astigmatism vs Myopia in children
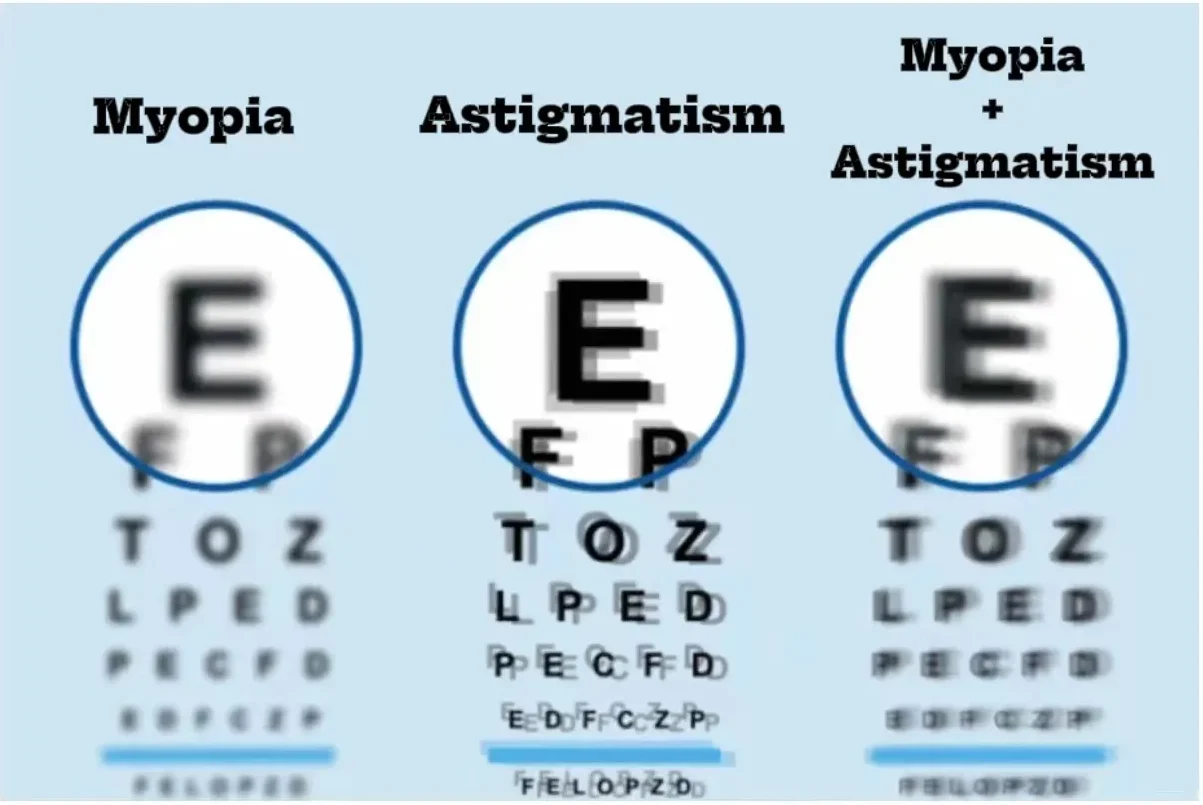
Vision comparison: Myopia – Astigmatism – Myopia with Astigmatism.
| Characteristic | Astigmatism | Myopia |
|---|---|---|
| Vision | Blurred both near and far | Blurred mainly when looking far, near remains fairly clear |
| Viewing posture | Tilts head, rotates notebook to “focus” | Rarely changes posture to see clearly |
| Associated symptoms | Headaches, eye strain, distorted text | Eye strain mainly with prolonged distance viewing |
| Impact on learning | Often misaligned writing, misreading | Difficulty seeing the board, but near reading is fine |
| Risk of amblyopia | High if untreated | Lower |
Diagnosis of astigmatism in children: what needs to be done?
- Autorefraction and visual acuity testing by age group.
- Corneal evaluation (curvature, axis) and cycloplegic refraction when needed to rule out accommodative spasm.
- Fundus examination to detect structural abnormalities.
Recommendation: Schedule eye exams every 6–12 months, or sooner if any signs listed in points 1–5 appear.
Treatment & orientation
- Cylinder glasses (astigmatism glasses): Correct astigmatic axis, improve clarity, prevent amblyopia.
- Toric contact lenses: Suitable for older children who can maintain proper eye hygiene; requires regular follow-up visits.
- Refractive surgery orientation when children are old enough & refractive error is stable:
- LASIK/SMILE: Applied if the cornea is sufficiently thick and has suitable morphology.
- Phakic ICL: An option for those with myopia combined with astigmatism (about 1–4D), thin corneas, dry eyes, or unsuitable for laser. Phakic ICL is a biocompatible lens implanted behind the iris, does not damage the cornea, and can be removed if necessary; provides clear vision both day and night for clinically eligible patients.

 vi
vi 27-Aug-2025
27-Aug-2025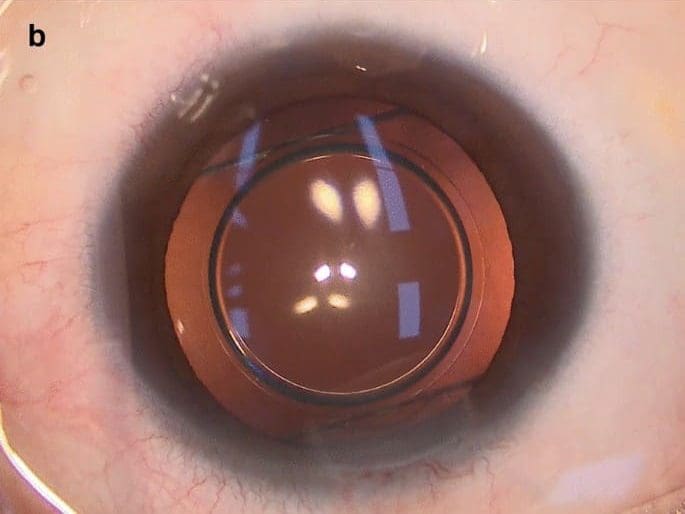










 0916.741.763
0916.741.763 Appointment
Appointment